What is Testosterone?
Testosterone is a hormone produced within the testicles via a joint process, which includes both the endocrine system and the pituitary gland. Testosterone serves as the male body's primary natural hormone, and is responsible for the proper development of male sexual characteristics. Although often referred to as a sex hormone, testosterone actually governs several areas within the body including a man's development from birth onward with responsibility for everything from determining gender, through pubertal changes and male potency (libido & sexual functioning), to the partitioning of bodily muscle and fat distribution. It is also an integral component in men's sense of well-being, playing a major role in your physiological, biological, and sexual health, while influencing stress coping capacity, sperm production, mental acuity (clarity, memory & recall, concentration & focus), bone density, immune system support, and red blood cell production. Of course testosterone is present in both males and females; however, males produce approximately ten times more than their estrogen-based female counterparts.
What Should Male Testosterone Levels Be?
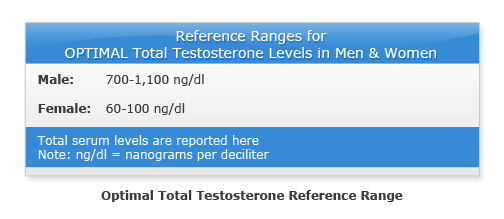
This chart is a good representation of what's considered the average upper and lower limits for testosterone in both males and females.

While the above ranges are considered average, they do not represent the optimal testosterone levels desired. For health and overall wellbeing, the following chart represents the reference ranges for optimal total testosterone levels in men and women.
Although normal male testosterone levels are primarily dictated by age, both genetics and lifestyle can be very influential factors, along with other external variables thus making any clear cut distinctions more difficult. However, men's testosterone levels generally breakout to approximate age and level figures of: 19-24, 700; 25-34, 658; 35-44, 617; 45-54, 606; 55-64, 562; 65-74, 524; 75-84, 471; 85-100, 376.
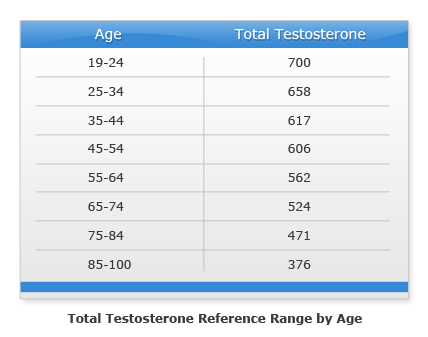
Generally speaking, as you age your testosterone level gradually declines at a rate of about 1 percent per year after age 30. So what if your levels are below normal? What is low testosterone, what does having it mean, and what can you do about it?
Low Testosterone in Men
Low testosterone rates are 'commonly reported' among today's middle-aged men, and constituted as a drop in testosterone levels below 350 ng/dl (nanograms per deciliter). Figures at or below the recognized bottom of the normal range were rarely ever reported in 1940's prior to age 80.
Generally speaking, testosterone levels rise rapidly throughout adolescence and peak in the early twenties, but there's a trend of decreasing serum levels that's occurring at earlier ages which is promoting greater incidences of low testosterone. Clinical estimates cite up to 50% of all 40 year old men now have testosterone levels below their age norm of approximately 620 ng/dl. The preponderance of research implicates pesticides and preservatives found in foods, along with the hormone pellets used to fatten pork, cattle, and chicken, which act as "hormonal disruptors" within the human body. It is also apparent that these disruptors are affecting both genders, and all ages. For example, they have been found to be equally as responsible for precocious (premature signs of) puberty in very young boys and girls, as for low sperm counts, infertility, obesity, and low serum testosterone levels in men of all ages. Of course not all low testosterone is attributed to such external factors.
Andropause is the popular term for the condition associated with the emotional and physical change men experience as they age. However, this condition goes by several aliases including late onset hypogonadism, male climacteric andropause, and androgen decline in the aging male (ADAM). Although traditionally attributed to aging, andropause is actually caused by a significant decrease in testosterone production, which results in diminished hormone levels. As expressed above, this naturally subtle decline in hormones begins around age 30 and progresses (at a rate of approximately one percent per year) until it reaches a substantial deficit sometime after age 60 (earlier for some, later for others). Consensus estimates cite the incidences of andropause in our society as follows: ages 40 to 49 at least 2% to 5% of men could be clinically diagnosed with the condition; ages 50 to 59 anywhere from 6% to 30%; ages 60 to 69 between 20% and 45%; ages 70 to 79 from 34% to 70% and; 80+ is at approximately 91%. Although the widespread normal ranges are often attributed to the different ways to measure androgens, and the various ways to define andropause, they are far more likely attributable to individual differences and sensitivities to hormonal shifts.
Regardless of whether your low testosterone production is the result of progressive andropause syndrome or other forces, the symptoms will be the same, and are characterized by:
- Decreased hemoglobin and possibly mild anemia
- Decline in energy levels, and participation in usual activities
- Increased visceral fat (between and surrounding internal organs)
- Reduced bone density which increases the risk of bone fractures, breaks, and osteoporosis
- Decreased lean body mass, accompanied by declining strength
- Changes in cholesterol and lipid values
- Decreased body hair (both amount and thickness)
- Changes in mood, which can manifest as irritability, depression, anger, and fatigue
- Decreased libido (sexual desire), and diminished erectile quality and overall performance
- Diminished body fat burning capacity
So what if low testosterone is present in the absence of advanced age, thus exempting andropause as its cause? When this is the case (barring other hormonal problems like a poorly functioning thyroid gland), the diagnosis is a condition known as hypogonadism, of which there are two types, "primary" and "central". In primary hypogonadism, the sex glands also known as gonads (testes in men) malfunction producing little or no hormones, the most common causes of which include:
- Viral infection
- Surgical history
- Kidney and liver disease
- Certain autoimmune disorders
- Genetic and developmental disorders
- Radiation treatment or exposure
- Chronic illness
- Chronic kidney problems or failure
- Cirrhosis of the liver
- Stress
- Alcoholism
- Obesity (especially abdominal)
- Rapid, significant weight loss
In central hypogonadism, one or both of the brain centers (hypothalamus and/or pituitary gland) which control the gonads is functioning improperly. The main causes of central hypogonadism include:
- Surgery
- Trauma
- Tumors
- Injury, infection, or loss of the testicle(s)
- Nutritional deficiencies
- Hemochromatosis (too much iron in the body)
- Chronic bleeding
- Certain medications, including steroids and opiates
- Genetic abnormalities such as Klinefelter's Syndrome (an extra 'X' chromosome)
- Chemotherapy or radiation treatments
- Inflammatory diseases such as sarcoidosis (a lung inflammation causing condition)
Testing for Low Testosterone
A blood test is used to measure the serum levels of testosterone, both bound (that which is attached to Sex Hormone Binding Globulin - SHBG) and 'free' (unbound) available testosterone. A deficiency is often denoted by a total serum level below 350 ng/dl. The blood sample should be drawn in the morning, because daily bodily stress (work, exercise, medication, etc.) can significantly influence testosterone production.
Measurements of FSH (follicle stimulating hormone) and LH (luteining hormone) are also evaluated and considered in the analysis, especially within men who complain of symptoms directly related to andropause.
Pre-Therapy Prostate Exam
Prior to testosterone replacement therapy, every male should undergo a prostate examination to both check and document the status of his prostate gland. Any abnormalities hypertrophy, or urinary complaints should be documented and attended to prior to commencing testosterone therapy.
It's often best to have both the physical prostate exam and the PSA (prostate specific antigen) blood test. Elevated PSA results are typically followed by a PSA II test, which may identify an enlarged prostate, a.k.a. prostatic hypertrophy. Testosterone replacement is absolutely contraindicated (to make a treatment or procedure inadvisable) in men with prostate cancer until cleared by a urologist.
Testosterone Replacement Therapy
Testosterone preparations, along with their prescribed dosages and frequency of treatment are medically customized for each individual into what is collectively known as hormone replacement therapy (HRT), or as testosterone replacement therapy (TRT).
TRT is a highly effective treatment regimen for specific testosterone deficiencies, andropause, and numerous additional causes of low testosterone production. However, there are times when certain pituitary gland problems require the surgical removal of a pituitary tumor, non-hormonal medication, radiation treatments, or the replacement of other bodily hormones.
Testosterone Preparations
Healthy testosterone production shows secretion throughout the day and night, with a peak in the very early morning hours. Ideal TRT would be administered in a manner which optimizes this natural secretion pattern. There are a variety of testosterone preparations, and several reasons to select one over another. For example, bodybuilders, other testosterone supplementing athletes, and even recreational users prefer testosterone injections to tablets because it permits them to avoid hepatotoxicity (liver toxicity) issues. This occurs during an oral steroid's initial trip through the liver (prior to entering the bloodstream to work), and is a process which both increases bad and decreases good cholesterol levels. Such users also favor injections because of the inherently short half-lives of oral medications, which cause them to both work and stop working rapidly, often requiring multiple daily dosing to maintain even blood serum levels. Nevertheless, each of the following options provides adequate levels of hormone replacement along with their inherent pros and cons. The trick is to find the one that best suits you and your style of living.
Oral tablets will always be en vogue because of their vitamin-like convenience and ease of use. Many men prefer this method not only because they're already accustomed to taking vitamins, but also due to their discomfort with needles. As mentioned earlier, tablets are harsher on the liver than other forms, and are generally taken daily or twice daily to ensure the proper dosage/stability throughout the day and night. For some though, they can also be too easy to forget, and would obviously not be a good choice for such men. These missed intervals often cause a roller coaster effect with varying testosterone levels and some patients only get a mild bump in there total testosterone elevation.
Another viable option is the testosterone patch. The patch comes in different dosages and brands, among which Androderm is probably the most popular. Although reportedly uncomfortable to some, most users are completely unbothered by it. The patch requires daily routine changing, similar to taking orals, yet it remains a popular delivery mechanism. Older versions of the testosterone patch were attached to the scrotum and genitals, but today's patches should be applied to a clean, dry area of the back, stomach, upper arms, or thighs. You'll have to rotate sites daily, allowing at least 7 days before reusing a site. Some people experience allergic reactions to the adhesive in the patch, which can manifest in a variety of skin irritations. Some patients after continued use have no response to the activity of patch and usually go to other delivery methods like cream or injections.
Intramuscular (IM) testosterone injections are shot directly into your muscle then absorbed into the bloodstream via the capillaries. IMs are not only popular because of their differing time release characteristics, but also because they don't disrupt liver functioning. IM testosterone therapy is generally esterified, which means that esters have been added to the preparation to control its speed of release and consequently, its rate of activity within the body.
There are four primary U.S. approved preparations:
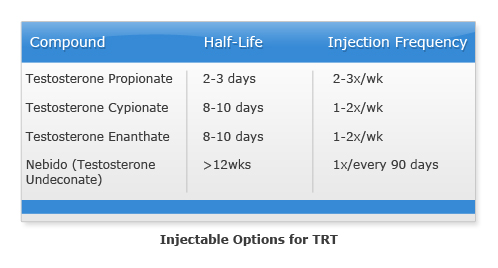
Other injectable preparations include hybrid blends of fast, moderate, and slow ester testosterones such as the wildly popular Sustanon 250, and its close relative Omnadren 250. These two products and other similar ones are optimally taken frequently early to benefit from the short esters, and then less frequently later once the long esters have accumulated within the bloodstream. This is popular because of the mutli peaks in testosterone over an extended period of time.
The testosterone gel or creams is prepared in various dosing solutions, and sort of melds together the characteristics of several applications. For example, it's absorbed transdermally (through the skin) like the patch, requires more frequent administration similar to tablets, and elevates serum levels quickly like both the aforementioned mechanisms and intramuscular testosterone propionate. Since its debut, testosterone gel has been a very popular preparation mostly because of its great convenience. However some patients only get a mild bump in there overall testosterone levels or none at all after a period of continued use and require a more effective delivery method like injections. Testopel, subcutaneous crystalline testosterone pellets, manufactured by Organon have been approved in the U.S. for the treatment of men with testosterone deficiency syndrome. These long-acting pellets are inserted subcutaneously (between skin layers), and can provide a sustained testosterone release for 3-6 months. Although not as popular as some of the other preparations mentioned these pellets are just as effective. Patients are required to undergo a surgical procedure to implant the pellets each time and the sensation of the pellets to some are annoying and bothersome.
Testosterone Boosters
Testosterone boosting is similar, but different from testosterone supplementation. For clarity, TRT/HRT uses synthetic testosterone preparations to actually replace the testosterone your body is unable to produce, while testosterone boosting works with your body (in most cases) to increase your naturally produced testosterone amount.
Chemicals
Said boosting can be thought of as having three primary categories. The first includes numerous present and former over-the-counter (OTC) chemical cousins like Havoc, Methyl-1-Testosterone, Superdrol, 1-AD, and numerous others which fall into the grey prescription drug/OTC supplement area. Although they all generate genuine testosterone increasing results, they were never FDA approved for, or sold as prescription medications. Admittedly, a good argument can be made for describing these products as testosterone replacements, but that debate is beyond the scope of this writing.
Herbal products
The second category is that of natural herbal testosterone boosters. Scores of supplement companies have made fortunes by producing entire lines of testosterone boosting products based on the centuries' old regional legends and reputations of such exotic testosterone enhancing herbs as:
- Eurycoma longifolia (commonly called tongkat ali or pasak bumi) a tall, slender shrub-tree native to Indonesia and Malaysia
- Lepidium meyenii, a.k.a. maca, an annual plant indigenous to Peru and parts of Bolivia
- Tribulus terrestris, without doubt the most popular, an herb that has been used as a traditional male reproductive medication throughout its native China and India for hundreds of years
Foods
Unlike synthetic boosters and supplements which can have negative side effects, the third category increases testosterone levels by employing specific foods and resistance training. The consumption of certain foods is known to increase testosterone.
Although generally considered a substance to avoid (for its tendency to promote plaque buildup within arteries) the body both produces its own, and requires the externally supplied consumption of cholesterol. Proven to increase testosterone levels, solid concentrations of cholesterol are often found within many of the protein-rich foods a fitness conscious person would normally consume anyway, like eggs and various lean red meats. Such foods provide great nutritional resources for your body as long they are consumed in moderation and kept lean.
Another low testosterone improving substance, which has also gotten a bad rap, is fat. Both the healthier mono- & polyunsaturated fats from olives, nuts, fish and seeds, and the unhealthy (in large amounts) saturated fats found in avocados, whole fat dairy products, and oils like butter and margarine work with the body to increase testosterone production.
The multi-faceted mineral Zinc is well-known for its ability to provide many bodily benefits including blood clotting, wound healing, tissue repair, immunity improvements, and bone health. But it is also a superb sperm and testosterone production boosting mineral. Zinc can be found in high amounts within oysters, beef, pork, turkey, chicken liver, and pumpkin seeds. Substantial, but lesser concentrations are in wheat germ, lentils, almonds, and sunflower seeds.
Resistance Training
Resistance exercise is an effective way to increase your natural testosterone production and sustain levels. In general, just working (moving) muscles very mildly stimulates testosterone secretion, but thoroughly taxed weight trained muscle release exponentially more testosterone. Obviously weight and cardio training are good for you on numerous levels, but it would be of great benefit to begin a serious training regimen if you're desirous of higher testosterone levels. More specifically, lower body training (especially programs which incorporate free-standing/universal bar squats), has been demonstrated to optimize weight trained testosterone release.
Additional Ways
Overweight men often have lower testosterone levels, so work to achieve a balanced body weight. The more stored fat you have, the greater your natural testosterone disruption. It is therefore advisable to shed any extra pounds you may be carrying in an effort to get closer to the weight established for your age, height, and build. Obesity not only reduces testosterone levels, it also elevates estrogen levels.
Never starve yourself when trying to lose weight. The consumption of too few calories inhibits testosterone production. Be sure to stay away from crash and fad diets - those that promise immediate results, and those that severely restrict macronutrients (fats, carbs, and proteins). Don't ignore carbohydrates because your body requires them for energy, just make smarter carb choices. Similarly, eliminating fats can cause a decrease in stored body fat utilization, and a plunge in testosterone levels. Try to maintain a balance between macronutrients, similar to the ratios found here: fats 15-20%; carbs 40-55% and; proteins 25-45%.
Don't permit long gaps between meals. Instead, try to consume 5 - 6 small meals a day. This will keep your blood glucose levels up (energy), help promote elimination (regularity), and help sustain optimal testosterone production. It's not easy to stick to a schedule during a busy work week, but if you can keep meals light, you'll naturally find yourself seeking food every 2.5 - 3.5 hours. Always have something quick and easy on hand like sandwiches, fruit, bars, nuts, shakes, lean cuisines, etc.
Alcohol consumption has been shown to adversely affect testosterone levels. If you drink, try to reduce your overall consumption, and try not to drink in a single sitting rather than throughout the day.
Low Testosterone in Women
Research has conclusively demonstrated that testosterone does effectively boost sex drive and resolve peripheral sexual problems within certain women with sexual dysfunction. Because estrogen is a woman's primary sex hormone, TRT is usually prescribed only for those women who have sufficient estrogen levels. Most physicians don't consider TRT appropriate for women who:
- Are post-menopausal
- Can't or choose not to take estrogen
- Have a history of breast or uterine cancer
- Have cardiovascular or liver disease
Studies have shown that TRT for women might be appropriate if they: are post-menopausal, receiving estrogen therapy, and have a decreased sex drive with no other identifiable causes and; have depression or fatigue after surgically-induced menopause and estrogen therapy has proved ineffective. TRT for women is most often prescribed in the form of a gel, patch, or cream. Oral tablets may be, but are rarely prescribed for women.
Although testosterone deficiency contributes to sexual dysfunction in women, other factors are more integral including: decreased estrogen levels; chronic health conditions; vaginal dryness; conflict; mood concerns; lack of emotional intimacy and; medication side effects. It should be duly noted that no commonly prescribed testosterone preparation has been approved by the FDA for female usage.
